Policy Makers Breakfast: The Time to Talk About Change
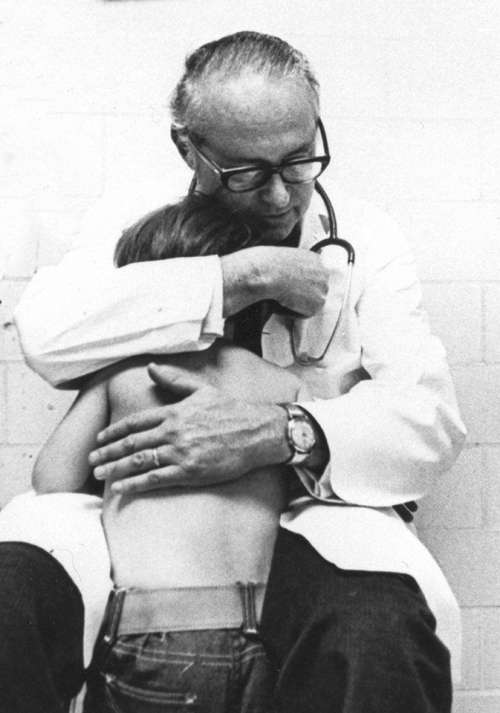
Policy Makers Breakfast: Honoring Dr. Melton The annual Uniting Communities Kempe Foundation breakfast on September 14 offered the opportunity to hear from Colorado General Assembly members, along with renowned advocates for the safety and wellbeing of children. This event and programs throughout the week honored Dr. Gary Melton who was a faculty member in the […]
Policy Makers Breakfast: The Time to Talk About Change Read More »